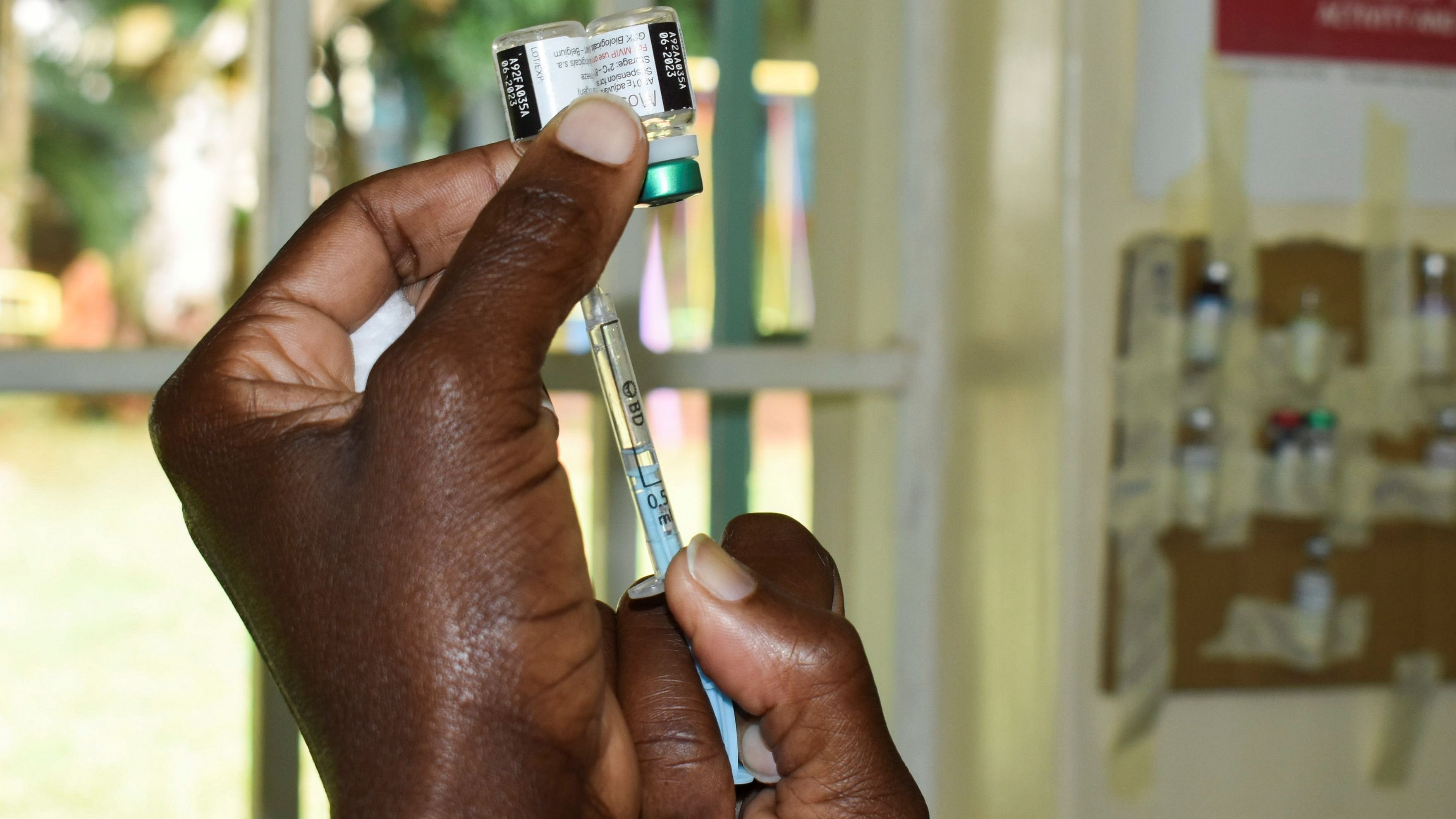
Some two decades after John Gallup and Jeffrey Sachs first estimated and documented the adverse severe deleterious effects of malaria for the economic development of nations, the world this last fortnight saw a malaria vaccine, Mosquirix, approved for the first time by the World Health Organization. Although an imperfect vaccine (other vaccines seem close competitors with better efficacy rates and close to approval), for the first time in humanity’s history, a disease that has afflicted humankind since the first millennium BC from Greece to China, and which the Italians named after bad air, seems to be heading towards eradication.
The timing could not have been better. It comes when the rich and poor world at the World Trade Organization (WTO) continues to disagree on the Covid patent waiver, and the weaknesses of the much-vaunted Covax programme stands exposed. Meanwhile, technologically, vaccine innovation goes through momentous leaps in mRNA platforms, such that Covid-19 had not only a vaccine approved with an unprecedented timeline of about a year, but also follow-on vaccines saw entries from other competing technologies and firms all over the world. We are also now seeing discussions on mRNA versions of Covid-19 vaccines coming from the developing world apart from conversations on Moderna getting in to trials for an HIV vaccine using the mRNA technology or how mRNA could give a new lease of R&D life to cancer vaccines.
Meanwhile, is the world under-celebrating the approval of Mosquirix? This should not be the case even if there is a policy paralyses with debates on a people’s vaccine for Covid-19 or booster doses or pediatric vaccines for the current pandemic. Not setting those important conversations aside, there are some key lessons for a new normal in the Anthropocene biopharmaceutical innovation from the Mosquirix approval. And primarily, it is this: perhaps it is finally time to ponder a social way in biopharmaceutical innovation.
But what is exactly a social way in biopharmaceutical innovation? The answer comes from who was behind the discovery of malaria vaccines. It was PATH, located in Seattle, Washington, registered in the 1970s and is a not-for-profit firm. They worked with the not-for-profit initiatives of GlaxoSmithKline and with funding from philanthropic entities like the Bill and Melinda Gates Foundation (BMGF). There are other vaccines and healthcare technologies PATH has been working on over the years, as their Wiki page reveals. But together in a social network with GSK and BMGF, they seem to have solved market failures around innovation in neglected diseases of the poorer world, like now, especially in malaria. Might other social solutions be forthcoming then if similar such partnerships are forged?
The second lesson to learn is the time taken to get a malaria vaccine approved, which has not been a year as we saw in the Covid-19 vaccine. The Mosquirix vaccine itself was first created in 1987. While perhaps the underlying technology was complex, it is also undeniable that apart from a couple of exceptions, few rich world biopharmaceutical companies or, for that matter, wealthy philanthropists cared enough to fast track solutions for the poor world’s diseases. Perhaps a social way, well forged and funded with a systematic R&D mechanism, can accelerate the time taken to launch a new vaccine tomorrow then?
The next lesson comes from the controversy around clinical trials around drugs and vaccines for neglected diseases. Even if you are not a fan of the Oscar-winning movie The Constant Gardener (strongly recommended, based on this trial location controversy issue), a cursory internet search will show that, for example, in malaria vaccines, most trial sites have been in Africa and South Asia, perhaps appropriately so given that these were the locations which bear the brunt most acutely from the disease. That said, there also have been controversies galore. PATH, for example, was in the docks in 2009-2010 for allegedly casually taking consent from thousands of trial participants for its HPV vaccine programme in Andhra Pradesh and Gujarat, two Indian states.
But here, one also must appreciate that clinical trials by some estimates account for about a third of the total R&D expenditure in biopharmaceutical innovation, and potentially social models would need to be smart about costs while choosing trial locations. One of the bigger constraints in the malaria vaccine programme has been funding, and this might be a larger constraint more broadly in a social way for biopharmaceutical innovation, a fourth lesson from the Mosquirix approval. The BMGF has over the years given more than $250 million for malaria vaccines R&D, but that is less than one-fourth of what the R&D expenditure looks like for an average new biopharmaceutical product ($1bn-$2bn according to some recent estimates). It is worth pondering if the malaria vaccines could have been fast-tracked with higher R&D financing, just like one has seen with Operation Warp Speed in Covid-19 vaccine using matching R&D money from for-profit biopharmaceutical companies. Perhaps that would also have taken care of the vulnerable not being recruited for clinical trial locations.
Finally, a reflection on heterogeneous business models under the broader ambit of social paths to biopharmaceutical innovation may be merited. There are now advanced market commitments to induce technology races as we saw for Covid-19 vaccines, crowd-sourced funding models of biopharmaceutical innovation, ideas around health impact funds or even open-source drug discovery models championed from low-cost innovation locations like India. That said, none seem to have raised enough money or have shown enough scientific promise to surmount the technological complexity that the PATH-way has been showing. A close similar model is the Drugs for Neglected Diseases Initiative. In this world that we live in with the potential aggravation of more incidences of zoonotic diseases in the Anthropocene tomorrow, perhaps then the time for the social-way for biopharmaceutical innovation has finally arrived.
Mosquirix is showing us a way for those willing to listen.
(The writer is a Reader in Economics of Innovation at the University of Sussex, Visiting Fellow at Hoover Institution, Stanford University and Visiting Faculty in Economics at IIM Ahmedabad, India)
Disclaimer: The views expressed above are the author's own. They do not necessarily reflect the views of DH.