Bipolar disorder is a complex and multidimensional psychological disorder. The key reason for its misdiagnosis is that bipolar disorder shares some of its symptoms with other mental conditions. That’s why the differential diagnosis of bipolar disorder is a must to rule out mental health issues that may have many similar symptoms.
Differential diagnosis
The following two mental disorders are the most shared differential diagnosis for Bipolar Affective Disorder (BPAD):
Recurrent Depressive Disorder: In the case of BPAD (Bipolar Affective Disorder - Bipolar 2), the most expected shared condition to consider is RDD (Recurrent Depressive Disorder). In a patient suffering from recurrent depressive disorder, the depression recurs even after treatment and keeps recurring. Here, the doctor must prescribe anti-depressants. Mood stabilisers may or may not play a role in this case.
Borderline Personality Disorder: It’s another mental health issue that is commonly confused with BPAD. Recurrent mood swings and anger outbursts characterise it. Depression is recurrent as well.
Factors leading to BPAD
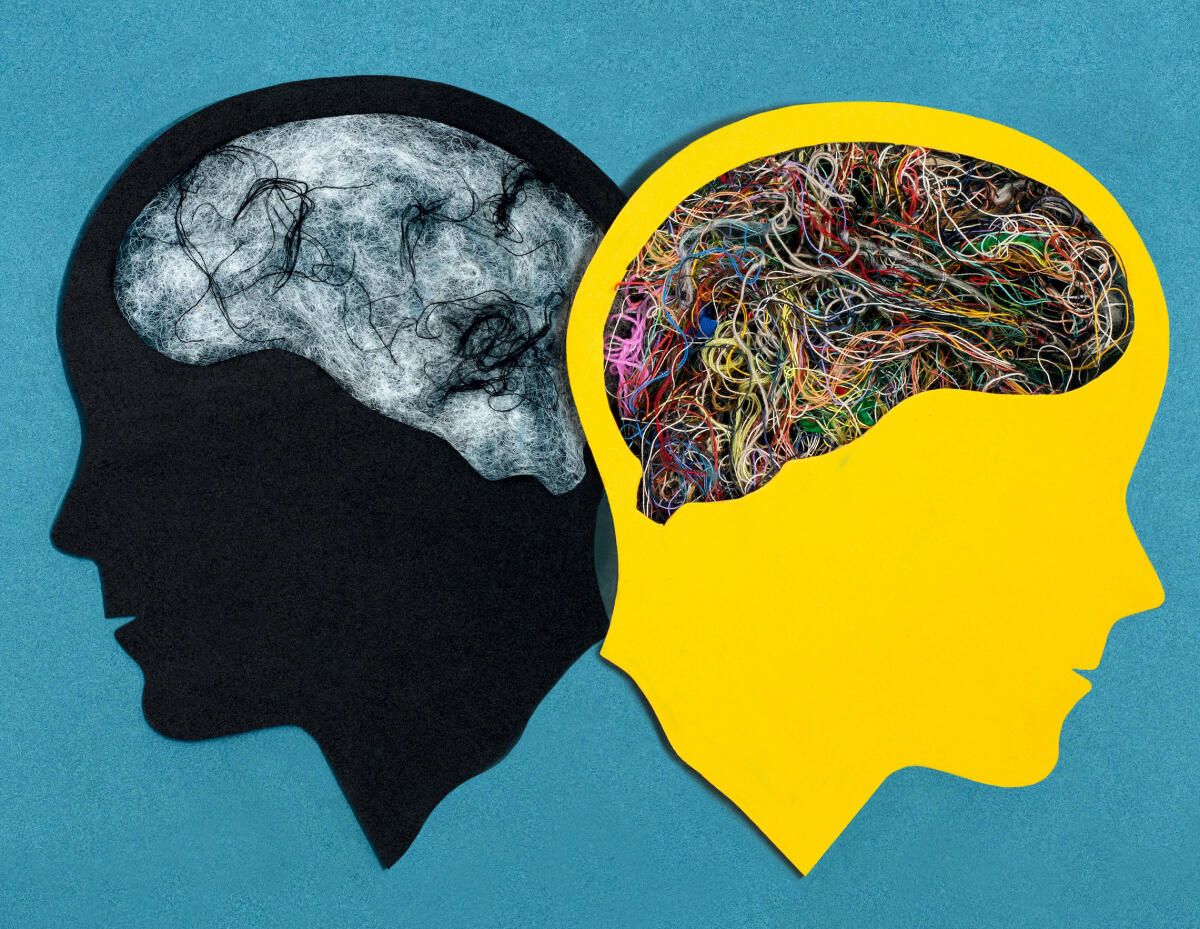
The exact causative data is not present. Rather, the final common pathway is known. There’s a disruption of neurochemical balance in the brain. A patient’s genetics also have some role to play. In a PET scan, certain changes are visible in bipolar patients. DWMD reading in a brain MRI scan is a classical sign in severely bipolar patients. In the case of the psycho-social model, childhood adversities do play a role in bipolar disorder. The genetic makeup of a person also plays a prominent role. The neurodevelopmental vs neurodegenerative hypothesis holds its ground here. So, biological and genetic factors play a significant role in this, while psychological adversities are contributory.
Dangerous signs
Is there a danger due to omitting information about hypomanic or manic episodes? Only the information about hypomanic episodes is at risk of omission. Frank mania is a medical or psychiatric emergency, depending on the severity. It is not managed on OPD-basis, and the patient has to be hospitalised. In hypomania, a patient can function well. They can go to the office and not suffer from psychotic thoughts. This episode lasts for 2-3 months, and relatives may omit it if they’re not vigilant enough.
In spite of medications, a person may develop mania or depression. The psychiatrist may up the dosages. A psychiatric phenomenon called kindling in the brain may get omitted. Kindling is like a seizure with electrical brain stimulations, and there may be convulsions. It can take place even though a patient is taking the prescribed medicines. The commonest cause for it, especially in India, is that patients refuse to take medicines after a few months. Once patients seem to improve, they refuse to take medicines for one reason or another, like the medicines have side effects, which can trigger mania.
Is there a need to change the course of treatment?
The course of treatment may need to be changed depending on the frequency of manic or depressive episodes. As their frequency increases, the doctor may go for more aggressive management. It includes giving more medicines and increasing the dosages of medicines. DWMD is a special finding in such patients upon an MRI brain scan.
There’s more brain damage; thus, a patient is prone to dementia. The lesser the frequency of episodes, the easier the functional management of a patient.
The social circle
Many people are vigilant when a patient is developing depression or mania. The social circle during the depression gets quite reduced. A patient is not able to interact when going through depression. In mania, hypersocial behaviour can be observed.
Most of the patients can maintain meaningful relationships if they take their mood stabilisers regularly. Though, their self-esteem needs to be taken care of as BPAD diagnosis, medicinal load, and self-image can take a toll. As BPAD is a major psychological disorder, other psychological aspects must also be considered.
It’s important to let the patient know they shouldn’t take major life decisions when going through mania or depression, like resigning from a job, making marriage decisions, etc.
(The author is a consultant psychiatrist with a leading Bengaluru-based hospital.)
Impact of differential diagnosis on treatment
Borderline Personality Disorder: Psychotherapy is one of the mainstays of treatment in this case. A patient is given mood stabilisers, antipsychotics, and anti-depressants, all three together. BPD is a person’s nature, and it mellows with time. After the age of 40, the problem may subside.
Bipolar Affective Disorder: A person must take medicines. Here, it’s necessary to
provide mood stabilisers or an antipsychotic with mood stabiliser potential.
Recurrent Depressive Disorder: Here, the doctor must prescribe anti-depressants. Mood stabilisers may or may not play a role in this case.
Bipolar-1 vs Bipolar-2: It’s very challenging to quote data on the misdiagnosis of bipolar disorder because its prevalence is only 1% in the population. People often confuse bipolar disorder with feeling depressed, elated, or irritated for some hours in a day. These symptoms can result from other issues like anxiety, depression or personality problems.
Bipolar-1: It is characterised by mania or expansive happiness. Patients feel like they know influential personalities and spend a lot of money, which lasts for months. There is classical depression in this case which can last for months as well. There could be multiple episodes of mania or depression.
Bipolar-2: It is characterised by recurrent episodes of depression. An episode of hypomania may occur in such patients once in a lifetime. It can only be observed if the patient’s relatives stay vigilant. It means that episodes of mania will become less frequent. A person will go to work, won’t get psychotic thoughts, and may seem energetic and interactive.