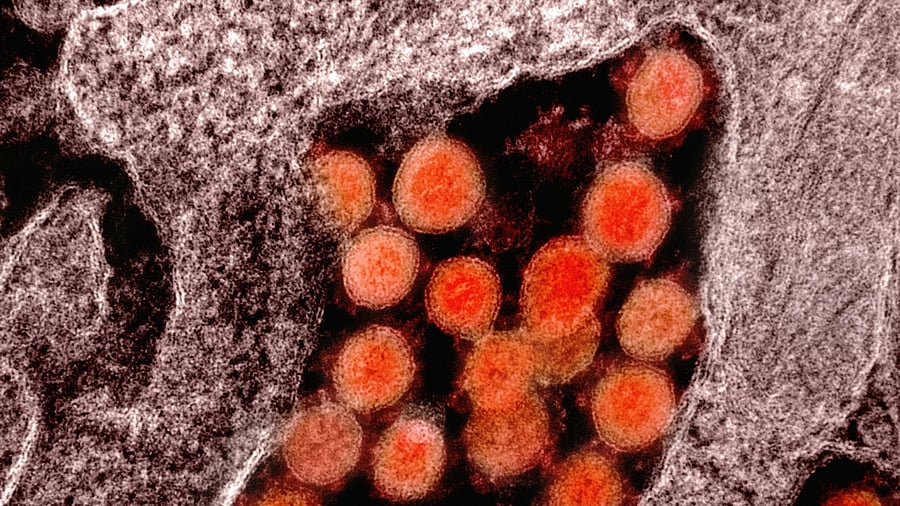
Image for representation, courtesy.
Credit: Unsplash photo
Transfusion-Dependent Thalassaemia (TDT) is a severe inherited blood disorder where the body cannot produce enough haemoglobin, making regular blood transfusions essential for survival.
Despite advances in treatment, a critical shortage of safe and compatible blood is worsening outcomes for patients, especially in low- and middle-income countries (LMICs). Many patients are unable to maintain adequate pre-transfusion haemoglobin levels, with some falling dangerously low. This leads to severe complications, including tissue damage, bone deformities, growth delays, and an increased risk of cardiac issues and early mortality.
What are the multifaceted challenges affecting blood transfusion support for thalassaemia patients, and what are the strategies for improving transfusion systems worldwide?
The root cause
In many LMICs, blood donation and distribution systems are often fragmented, relying on local hospitals or family members as replacement donors. This disjointed approach undermines blood inventory predictability and poses safety risks. Additionally, logistical inefficiencies, such as inadequate cold-chain infrastructure, often lead to wastage and delays.
Inadequate blood matching
Transfusion-dependent patients face heightened risks of developing alloantibodies (immune responses to foreign red blood cell antigens). Inadequate blood matching — beyond basic ABO and RhD typing — can lead to complications like haemolytic reactions, which affect up to 30% of patients in some regions.
Limited advanced blood safety technologies
In high-income countries, advanced technologies such as Nucleic Acid Testing (NAT) and pathogen inactivation are used to ensure blood safety. Unfortunately, these technologies remain inaccessible or underused in many parts of the world, resulting in a higher risk of transfusion-transmitted infections like hepatitis and HIV.
Lack of national blood policies
Many countries lack comprehensive national blood policies, which hinders the establishment of quality controls and haemovigilance systems. The absence of centralised registries for rare blood donors also makes it difficult to match patients with compatible blood, especially for those with rare genetic profiles.
External factors add to the crisis
The Covid-19 pandemic had a profound impact on global blood donation systems. In regions like Gujarat, donations dropped by up to 50%, severely affecting transfusion schedules for Thalassaemia patients. Mobility restrictions, fears of virus transmission, and vaccine deferral policies led to dangerous delays in care.
Natural disasters & conflict
Regions affected by conflict or natural disasters, such as Syria or Yemen, often experience complete breakdowns in blood transfusion systems. Damage to hospital infrastructure, shortages of fuel, and disruption of supply chains make it almost impossible to deliver timely and safe blood to those in need.
Strategies for better services
Addressing the blood supply crisis requires systemic reforms, as well as innovative community-based solutions. Here are several strategies that can significantly improve blood transfusion care:
Centralised blood collection systems: Centralising blood services can standardise donor screening, blood collection, and inventory management, ensuring better safety, efficiency, and reliability. Countries like the UK and Singapore have successfully implemented such models, improving blood safety and availability.
Encouraging voluntary donors: A key strategy for ensuring a reliable blood supply is the promotion of voluntary, non-remunerated donors. Programmes like Turkey’s “Blood Mother/Blood Father” initiative have shown success in mobilising community support, ensuring sustainable donor pools for Thalassaemia patients.
Advanced blood matching & donor registries: Introducing extended red cell phenotyping and molecular genotyping can pre-empt alloimmunisation and improve donor-recipient matching. National registries for rare blood types are also critical for ensuring that all patients, especially those from minority ethnic groups, have access to suitable blood donors.
Strengthening haemovigilance & legal frameworks: National haemovigilance systems — monitoring the safety and outcomes of blood transfusions — are essential for identifying adverse reactions early. Legislation that mandates safety standards and protocols across blood banks would ensure consistent and reliable care.
Digital transformation & AI: Digital tools that track blood donations, patient histories, and inventory levels can improve efficiency and reduce shortages. Predictive logistics powered by AI can help forecast demand and optimise resource allocation, ensuring blood supply is always available when needed.
Public education & awareness campaigns: One of the main barriers to consistent blood donation is misinformation. Public campaigns that promote the safety and importance of blood donation — especially in the context of post-vaccination or other misconceptions — can encourage more people to donate, thus stabilising blood supplies.
Transfusion-dependent Thalassaemia remains one of the most pressing global health challenges, exacerbated by systemic inefficiencies, a lack of infrastructure, and chronic blood shortages. While advances in gene therapy and synthetic blood products offer hope for the future, the immediate need for safe, reliable, and sustainable blood transfusion services is undeniable. Governments, health organisations, and communities must work together to ensure that every Thalassaemia patient receives the life-saving care they need.
Some CRISPR solutions
Synthetic & alternative blood products: Research into synthetic blood products, such as haemoglobin-based oxygen carriers and lab-grown red blood cells, holds potential for addressing supply shortages in the future. However, these technologies are still in their infancy and face significant challenges in terms of cost and scalability.
Gene therapy & curative solutions: Gene therapies, including CRISPR-based gene editing, are showing promise as potential cures for Thalassaemia. While these treatments have demonstrated success in clinical trials, their high cost and limited availability mean that blood transfusions will remain a cornerstone of Thalassaemia care for the foreseeable future.
International blood-sharing networks: Global collaborations and regional blood-sharing frameworks can help alleviate shortages in countries facing chronic deficits. A coordinated effort to harmonise safety standards and establish cross-border agreements could bolster blood transfusion systems and ensure no patient is left without the care they need.
(The author is the head of paediatric haematology, oncology, clinical immunology, and bone marrow transplantation in a leading Bengaluru-based hospital.)