Credit: Special Arrangement
A pilot recently consulted dietitian Edwina Raj after his endocrinologist prescribed Mounjaro, a diabetes drug also known to aid weight loss. Her task was to design a nutrition plan for him. “He was pre-diabetic. Because of long working hours and limited access to home-cooked meals, he struggled to make lifestyle changes to manage his weight. That’s why the doctor put him on the drug,” she says.
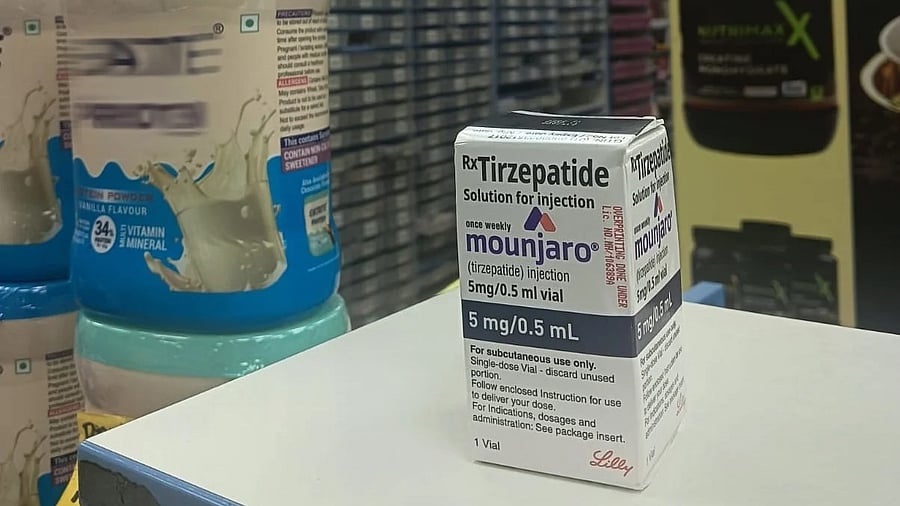
Doctors in Bengaluru are prescribing injectable drugs like Mounjaro (tirzepatide) and Wegovy (semaglutide) to patients unable to sustain their weight-loss efforts. But though the medication accelerates weight loss, they say it must still be paired with healthy eating and exercise to prevent muscle loss, and requires “mental preparation” to cope with side effects such as nausea and constipation.
Challenges
Edwina recalls a cautionary case. A woman with fatty liver issue lost 12 kg in four months after an online physician prescribed a weight-loss drug for her obesity and PCOS, which were affecting her fertility chances. But she also suffered severe hair fall and muscle loss. Her gastroenterologist eventually recommended she get a nutrition plan to help her lose weight safely. According to Edwina, a common mistake people make is that once their appetite drops, “they stop focusing on the quality of their food, which leads to a deficiency of macro and micronutrients”.
According to, Dr Chitra Selvan, professor and head of endocrinology department at a medical college, these medications work by inducing a feeling of fullness and slowing stomach emptying (a process by which food moves from the stomach to the small intestine). This reduces appetite and also food intake. But Dr Naresh Bhat, gastroenterology and hepatology expert, says about a third of his patients cannot tolerate the fullness and accompanying nausea. “In two or three cases, the medication had to be stopped,” he says. He emphasises the need to counsel patients first, by walking them through questions like ‘What does it do?’, ‘What to expect?’ or ‘What side effects can happen?’. “Otherwise they may stop taking it,” he explains.
Consultant dietitian Jayashree Bafna recalls a referral from an endocrinologist. The woman, in her late 20s, was mildly obese, pre-diabetic, and had thyroid complications. She was put on a weight-loss drug. “I suggested balanced one-pot meals and snacks like khakra, roasted chana, makhana, and buttermilk. But she did not follow through and later complained of heaviness and stomach pain. She has not returned.”
Endocrinologist Dr Mahesh D M cautions that people with delayed gastric emptying or poor digestion may experience side effects. Patients are, thus, usually advised to try the drug for at least a month (weekly doses) and their response is reviewed.
Dr Chitra adds that discontinuing these medications can also lead to some weight regain.
Then there is the cost factor. Mounjaro (5 mg, 0.5 ml solution) costs around Rs 4,000, while Wegovy, a pre-filled injectable pen, is priced at about Rs 16,000 per pack. Ozempic (semaglutide) has been approved for adults with type 2 diabetes but isn’t available in the Indian market yet.
Right candidates
Dr Chitra says while this class of medications has long existed in the Indian market, the newer formulations have been designed in doses that primarily promote weight loss. The recent approval of these molecules for weight loss even in individuals without diabetes has led to a greater visibility and buzz around them now, she explains. “Such drugs are meant for people with obesity (BMI of 30 kg/m² or more) or those who are overweight (BMI between 27 and 30 kg/m²) and have Type 2 diabetes, hypertension, heart disease, sleep apnea, or fatty liver,” she says.
Dr Bhat weighs in on the craze: “With bariatric procedures, you can lose significant amount of weight. Exercise can help you lose small amounts of weight. With these medicines, you can lose 8-10 percent of weight over time.”
Dr Mahesh has prescribed Mounjaro to both diabetic and non-diabetic patients — including those who gained weight during the pandemic or after pregnancy. He says portion control is key on this journey, but some struggle to adjust. “Two of my patients continued eating out of habit despite feeling full and ended up vomiting. If half a chapati makes them feel full, that’s where they should stop,” he says. He also advises such patients to drink at least two litres of water daily and avoid aerated drinks, fried foods, and alcohol.
Dr Srinath Aswathiah, an endocrinology expert, has prescribed such drugs to a range of obese patients — non-diabetics, pre-diabetics, and diabetics. His patients have not requested him to put them on these medications, but only enquired “out of curiosity”. However, he doesn’t start them on these drugs immediately. “We first encourage them to manage weight on their own. Based on their motivation and response, we discuss possible side effects and then decide,” he says. He considers starting the drug when lifestyle or metabolic issues limit weight management.
Still skeptical
In the past three months, IOC sports nutritionist Deepika Vasudevan has been approached by six people seeking prescriptions. “When I explain that I am not authorised to prescribe it and outline the risks, some ask for supplements instead,” she says. One man, however, was insistent. “He didn’t believe in nutrition plans. He wanted a quick fix because he had been chubby since childhood,” she says. Most others were women hoping to shed post-pregnancy weight. The fear in the medical fraternity is that injections such as Ozempic and Mounjaro could become ‘vanity drugs’, used for cosmetic rather than health reasons. But not too many are demanding the injections for weight loss. The steep prices and fear of side effects may be holding people back. One pre-diabetic woman, for instance, changed her mind about taking a weight-loss drug after reading about potential side effects and instead approached Edwina to make amends to her lifestyle.
Deepika has come across high-net-worth individuals who have tried these medications. “The rapid weight loss leads them to seek skin-tightening procedures to address sagging as they lose a lot of muscle. But even suddenly switching to a high-protein diet to regain muscle can cause gut issues. So eating right while working on prevention of muscle loss is important,” she says.
According to Aswathiah, patients can lose 6-8 kg in the first or second month, though some regain weight if they stop. “However, many decide for themselves that their current weight loss is enough and discontinue. Each patient responds differently,” he notes.
Grey areas
While interest is high on social media, Dr Bhat says key clinical questions remain. “We still don’t fully know who should take it, for how long, and how to manage the side effects. We prescribe in cases of fatty liver, to prevent progression. If you use that on someone who's obese, who's got fatty liver and even diabetes, we can reverse some (conditions). But if the disease has progressed to cirrhosis and you keep giving this, it’s a waste of time and is also dangerous,” he explains. Dr Bhat also flags the increased risk of gallblader stones as another side-effect.
Dr Praveen Kumar, clinical pharmacologist, warns that as demand rises and prices fall, unsupervised use could become widespread, potentially replacing the role of traditional lifestyle management such as having a balanced diet. “Poor eating habits can increase the risk of cardiovascular disease,” he adds.
To curb the possibility of self-medication, Jayashree demands stricter regulations so these drugs aren’t easily available without prescription.
And Dr Aswathiah stresses the need for doctors to stay updated through medical conferences and research before prescribing. He is also concerned about the misuse by non-medical practitioners with limited understanding. “Patients should take these drugs only after knowing the potential complications,” he cautions.
Reality check
All these are prescription medications. For a reality check, Metrolife visited pharmacies and also tried ordering these weight-loss drugs online. They refused to dispense the medication without a prescription. For the online order, we opted for the free online consultation to get a prescription. A caller on the other end claiming to be an internal medicine specialist assessed our BMI over the phone (no video check) and cancelled the order after deeming us ineligible.
Dr Kumar says, “A valid prescription must carry the doctor’s name and registration number.”
Experts welcome such prescription checks but urge further safeguards. Dr Bhat notes that some firms now insist on prescriptions from endocrinologists or subspecialists, while Dr Chitra stresses that the first consultation should always be in person and with an endocrinologist. “We measure waist, height, and weight, and review the medical history before prescribing these medicines. We also assess risks for complications, set realistic goals, discuss remedies for common side effects, and teach injection technique to ensure safe and optimal use of these medications,” she says.